The appearance of flesh-colored conical growths in the genital area is a reason for concern, which is fully justified, because the health of the genital area is an important point for the overall physical and moral well-being of a person.
These warts cause discomfort, interfere with normal sexual life, and can cause more serious health problems. If the integrity of the condyloma is damaged, infection and transition to a malignant formation may occur. Therefore, the desire to get rid of such manifestations is understandable and quite natural.
Reasons for occurrence
The causative agent of nipple papilloma is the human papillomavirus. This virus contains a specific set of DNA that successfully integrates into the cells of the human body and causes them to change their developmental cycle, shape and structure.

According to the international classification of diseases ICD-10, the human papillomavirus has the code B97. 7. Anogenital warts of a venereal nature have code A63. 0.
There are many different strains of this virus, each of which causes specific wart papillomas. The type of virus determines the course of the pathological process, symptoms, place of manifestation and severity of complications.
Strains are divided into two main types:
- cutaneous, with a dominant appearance on the dermal layer;
- mucous membranes, which appear on the mucous epithelium of the genital organs, oral cavity, etc.
In addition, the types of papillomavirus differ depending on the risk of degeneration into an oncogenic process into oncogenic, moderately oncogenic and non-oncogenic.
In the body of an infected person, several different strains are most often present at the same time.
Routes of infection and risk factors
There are several ways for a pathogen to enter the body:
- "Vertical" transmission. This is the name given to the transfer of an infectious agent from mother to child during pregnancy. Currently, it is not known whether the infection occurs in the prenatal period or directly during childbirth, but it is undesirable to perform a caesarean section in a mother with papillomavirus. Cesarean section is chosen only in case of bleeding papilloma inside the birth canal.
- Sexual way.An infectious agent can enter the body during vaginal, oral or anal sex. The pathogen is also transmitted by saliva during kissing. Using a condom during sex does not guarantee protection against the virus, but it does make its transmission less likely.
- Household.This mechanism of disease transmission is quite rare. Infection can occur through contact with the patient's personal belongings. Since the virus is found in saliva and urine, it is possible to get infected by using other people's dishes, shared towels, personal hygiene products, from the edge of the toilet or in the bathroom.
The mode of infection is mainly determined by the age of the person: in infants it can be determined with a high degree of certainty that the infection came from the mother, and in older children through contact and contact in the household. From the age of 17, sexual transmission occurs in most cases.
According to statistics, the human papilloma virus is present in the bodies of more than half of the sexually mature population, but in most cases it does not manifest itself in any way and is present in the form of a carrier.
The peak of the disease occurs at the young age of 17 to 25 years. This is due to maximum sexual activity and high sensitivity of the epithelium on the organs of the genitourinary system.
Predisposing factors that increase the likelihood of the disease are:
- early onset of sexual activity;
- frequent change of sexual partners;
- age up to 25 years;
- sexual contact with persons who previously had the human papillomavirus or other sexually transmitted diseases;
- pregnancy;
- imbalance of intravaginal flora;
- any chronic diseases;
- endometriosis;
- therapy with cytostatics or glucocorticosteroids;
- excess weight;
- thyroid gland disorder and insulin production disorder;
- hypovitaminosis.
Frequent stress and non-observance of the principles of personal hygiene greatly increase a person's chances of an infection entering the active phase after entering the body.

After ingestion, the virus spreads throughout the body through the bloodstream, binds to cells, penetrates their structure and integrates its DNA into the cells' DNA. The affected cells then begin to actively grow and divide, which is why condylomas appear.
Ways of development
After entering the human body, the virus does not cause any symptoms for a certain period of time.
The course of the disease proceeds according to the following algorithm:
- Hidden period. At this stage, the carrier is not aware of the presence of an infectious pathogen, because there are no clinical manifestations. However, at this stage the person is already contagious and can infect their partner through sexual contact. This latent period can last from 2-3 months to several years.
- The appearance of the disease occurs when the virus multiplies sufficiently in the body or when the protective mechanisms of the immune system are reduced. During this period, the first symptoms appear.
- Active development with increased symptoms.
The further course of events develops in one of the following directions:
- self-healing with the complete disappearance of nipple papillomas (most often observed after the end of pregnancy);
- slow flow and lack of growth of skin growths;
- active dynamics of papillomas with an increase in shape, size, number and merging of closely located groups;
- degeneration of benign growths into malignant ones.
Types of condyloma
There are several conventional types of condyloma papilloma:
- exophytic- protruding above the surface of the skin or mucous membrane with desirable outward growth;
- endophytic- with dominant ingrowth deep into the skin structures, which is why it is barely noticeable during visual inspection;
- Buschke-Levenshtein education- characterized by rapid growth, large sizes and frequent relapses after treatment. In this form, there is external growth and damage to the deep inner layers of tissue.

Genital warts can have a thin base or a wide base in shape. If the stem is thin, the tip may be sharp or club-like. Broad-based papillomas are quite rare. The color of all such growths is close to the color of the skin: from flesh to pink. The surface can be soft or covered with a layer of keratin.
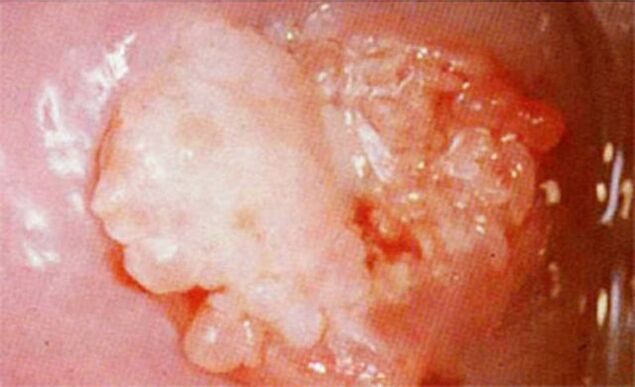
Warts can appear singly or in groups that look like nodules. Sometimes such multiple groups reach a size of 1. 5 cm. When several groups merge, formations appear that resemble cauliflower florets or a rooster's comb. These growths facilitate the identification of the disease after examination.
Individual growths usually do not cause as much discomfort as large elements. In rare cases, they crack and bleed slightly.
Large formations are more problematic: they can soak, bleed and worsen due to secondary infection that takes root in the affected areas.
Symptoms
The first symptoms appear after the end of the latent period, which in the shortest case lasts several weeks.
The appearance of condyloma occurs as follows:
- slight redness appears on the skin, which begins to itch;
- a rash in the form of bubbles or small bumps appears on the surface of the skin or mucous membrane;
- tubercles gradually increase to 1-1. 5 centimeters in length;
- New rashes appear nearby, which also turn into condyloma papules.
Localization depends on the specific strain and the place of entry of the pathogen into the body:
- external genitalia;
- anal area (anogenital papillomas);
- inside the urethra;
- on the cervix;
- on the epithelium in the mouth (on the buccal surfaces, tongue and inner side of the lips).
The clinical picture may differ in each specific case depending on the person's state of health. For small warts, no other symptoms can be observed.
With a more severe flow, the following accompanying symptoms are observed:
- itching or burning at the site of the rash;
- sensation of a foreign body in the perineal area;
- humidity in the area of neoplasms;
- unpleasant smell from the area where the warts are located.
With physical activity, long walking or running, all the above symptoms are intensified.
In severe cases, fatigue, weakness, signs of intoxication, long-lasting headache, fever and high temperature are observed.
In men and women, the symptoms have certain differences. This is due to anatomical differences and characteristics of sexual behavior.
Manifestations in men
Condylomas in men most often affect the scrotum, groin, pubis and various structural parts of the penis: glans, body, frenulum and prepuce, coronary groove. When localized near the urethra, papillomas acquire a pronounced red color, and this location often causes the stream to fork or spray when urinating.
If the rash is located at the exit from the anus, severe pain may occur during bowel movements, and blood may be present in the stool. Because of this, there is often a reflex fear of defecation, which causes periodic constipation and sometimes hemorrhoids.
There is often a vague pain in the lower abdomen, burning and pain during sex, as well as when urinating.
Long-term presence of infection reduces a man's immunity, making him more susceptible to respiratory diseases, which are more difficult to treat than usual.
Manifestations in women
The most common places for the appearance of papillomas in women are the perianal zones, where humidity and temperature are constantly increased: the epithelium of the clitoris, the labia, the vaginal outlet and the opening of the urethra. If an infection occurs during anal sex, a ring of growths may be concentrated around the anus.
Large growths often become secondarily infected, causing a strong odor, bleeding, ulcers, and severe pain when touched. When walking, irritation and severe discomfort is observed.
In 50% of women, whitish elements are formed on the cervix, which is detected by a routine colposcope, before which they are treated with an acidic disinfectant that can intensify the white color of the condyloma.
In some cases, all growths are located on the mucous membrane of a woman's internal genital organs, so she does not notice them until the scheduled visit to the gynecologist. This is often the reason for starting treatment later than in men.
Often, women experience discomfort due to the presence of formations in intimate places, which forces them to refuse sex.
Rarely, papillomas appear in the mouth, and in extremely rare cases - on the pubis, thighs, neck or face.
Characteristics of condylomatosis during pregnancy
If condylomatosis has been treated, pregnancy should be planned for a few months at the latest. The period of abstinence from pregnancy is extended if the woman took antiviral drugs during the therapy. After successful treatment and maintained interval, you can safely get pregnant.
If the disease is detected already during pregnancy, it is recommended to wait for treatment until all the baby's organs have already formed. Treatment after 28 weeks does not cause developmental abnormalities in the fetus.
The reasons why condylomatous warts appear in pregnant women include a standard decrease in immunity with increased stress on the body and significant hormonal fluctuations.

If papillomas are located on the external parts of the genital organs or in the perianal area and do not cause discomfort, then the issue of treatment can be postponed until the birth of the child. But in case of rapid growth, increase in size and severe pain in growths, consult a doctor immediately. Sometimes, with a high rate of progression of formations, their loosening is observed, which can lead to rupture of the vagina.
This disease, as a rule, does not affect the formation of the fetus, but its effect extends to the condition of the mother and the process of childbirth. If other infections are present, there is often a risk of premature birth.
When the condylomas are damaged during the passage of the fetus through the birth canal, it often leads to infection of the baby and condylomatosis of the larynx in the neonatal or thoracic period. Therefore, the presence of significant papillomas in the birth canal is a direct indication for cesarean section.
If necessary, the growth is removed during pregnancy, after which the tissue is sent for histology to confirm its benign nature.
The use of traditional medicine methods to remove condyloma during pregnancy is unacceptable, because it can not only not have a positive result, but can lead to the degeneration of benign cells into malignant ones.
Formations that did not cause discomfort during pregnancy often disappear on their own without treatment within a few months after childbirth, as the woman's hormonal balance normalizes.
Diagnostics
If the patient notices symptoms reminiscent of the human papillomavirus, then he should consult a gynecologist, urologist or venereologist.
First of all, the expert conducts a survey to clarify the following points:
- time of discovery of the first symptoms by the patient;
- probable causes of infection;
- dynamics and development of the disease until going to the doctor.
After that, a clinical examination is performed, during which the specialist determines the location, intensity, size and condition of the growths. For women, additional colposcopy (examination of individual genital organs with magnification) or extended colposcopy (similar procedure using acetic acid solution) is performed.
For a more accurate diagnosis, the doctor prescribes the following additional tests:
- PCR diagnostics, allows you to detect the pathogen in scrapings from the epithelium of the affected areas and determine its quantity (it also allows you to determine the strain of the virus);
- anoscopy- visual examination of the area near the anus with magnification;
- cytology and histologyfragments of formations for identification of atypical cells or tissues;
- biopsy of growthsfrom epithelial tissue for microscopic study of tissue structure;
- antibody titer detectionto this virus;
- smearfrom the cervical canal and cervix for microscopic oncocytology.

If necessary, consultations with a dermatologist or proctologist are scheduled. If the diagnosis is performed on a pregnant woman, then it is necessary to contact an obstetrician-gynecologist.
After receiving all the necessary data, the specialist can choose individual tactics for therapy and complete relief from the disease.
Treatment
Often, with condylomatosis, people avoid going to medical institutions and choose therapy themselves, giving preference to local drugs that can remove visible manifestations, but do not treat the body of the infection, transferring it to the latent phase. Such treatment almost always leads to relapse. Therefore, the final cure requires an integrated approach, which can only be determined by a specialist.
Treatment is carried out in the following areas:
- removal of growths;
- fight against viruses;
- strengthening the patient's immunity.
All methods used in the fight against genital warts are divided into radical and medical.
Radical methods
Such methods are chosen if it is necessary to urgently eliminate external manifestations or when condylomas are localized on the cervix in women.
The following methods are used for removal:
- Surgical excisionformations using a scalpel under local or general anesthesia. The incision site is sutured with surgical thread. Despite the fact that this method is considered classic, it often causes postoperative bleeding and long-term rehabilitation in the hospital, so recently surgical removal has been used less and less.
- Cryodestruction with liquid nitrogen.This method is relatively cheap and safe and does not require anesthesia or anesthesia. After freezing, the protein formation is destroyed, the nodules dry up and fall off. After a few weeks, no scars or scars remain at the treatment site.
- Laser removal.Despite its safety and high efficiency, the method requires anesthesia and is characterized by a high price, so it is prescribed if other methods cannot be used. When exposed to the laser beam, the structure of the growth stem is destroyed. After cauterization, the condyloma is deprived of nutrition, which within a few days leads to its necrosis and the scab disappears. Scars often remain after laser removal.
- Electrocoagulation.The method is affordable, but very painful, so local anesthesia is required. Genital growths are exposed to high temperatures, during which the papillomas are cauterized. The scabs fall off on their own after a few days, leaving behind scars.
- Radiosurgery.At the moment, this is the most modern, fast and effective method, which determines its high price. Using high-frequency radio waves, genital warts are painlessly removed in 15-30 minutes. After such removal, there is no bleeding, healing occurs within a day, after which no traces remain on the skin.
- Destruction by chemicals.This technique is only suitable for small formations, without multiple fusions. Special strong substances are used, which leads to the death of growth cells. These products are based on high concentrations of acids or alkalis that cause local chemical burns.
If we limit ourselves only to radical methods of combating condylomatosis, then recurrence of condyloma occurs in every third case.
Drug therapy
An integrated approach includes the removal of benign formations, getting rid of viruses in the body and increasing the immune status. Therefore, drug treatment includes the use of such drugs:
- Pharmaceutical productsfor nipple necrosis, acceptable for home use. For several days, this product should be applied pointwise to the warts. If the drug gets on healthy tissue near the growth, a deep chemical burn will be created, so you must apply the drug very carefully. After daily applications, take a short break of a few days. If the shoot does not fall, the course is repeated. Pharmaceutical products that cause growth necrosis include solutions and ointments.
- Antiviral agents.They can be for local or systemic use.
- Immunomodulatorsto improve immunity.
In addition, to improve the body's defenses, systematic intake of multivitamin complexes, a special diet and a healthy lifestyle are prescribed.
After treatment, immunity to condylomatosis does not develop, so re-infection from a previous sexual partner is possible.
Possible complications
If left untreated for a long time, condyloma causes the following complications:
- Binding of bacterial infection to damaged condylomatous papillomas, which leads to purulent formations, balanoposthitis and ulcerations in the perianal area.
- When growths grow in the urethra, viral-bacterial urethritis can develop, leading to problems urinating, urinary retention, and urinary tract infection.
- When large formations are localized in the anus, hemorrhoidal bleeding and paraproctitis occur.
- Genital warts can affect a person's sex life, causing them to refuse sexual intercourse. All this often leads to depression and psychological problems.
- Women may develop cervical erosion and dysplasia.
- The biggest danger is the risk of benign tumors degenerating into cancer (cancer of the head of the penis or cervix).
Preventive measures
Prevention of condylomatosis is divided into specific and general.
Specific preventive measures include vaccination with the new quadrivalent vaccine. These vaccines do not work against all strains of human papillomavirus, but they successfully fight against the most dangerous of them, which cause cervical cancer. Vaccination is carried out from the age of 11 and is repeated three times.
Non-specific prevention is similar to the measures inherent in many sexually transmitted diseases:
- use of protective contraception;
- personal hygiene at an appropriate level;
- regular sexual partner;
- regular examinations with a gynecologist or andrologist;
- timely treatment of diseases of the pelvic organs;
- giving up alcohol and smoking.
In addition, it is necessary to avoid stress, physical fatigue, hypothermia and all factors that weaken the immune system. A healthy diet, improved health and proper sleep patterns will help prevent genital warts.














































































